The COVID-19 pandemic reshaped lives around the world. Isolation from friends and family, fear of contracting the virus, threats to job security, overhauls of daily life, and constant adjustment to a developing crisis brought many unexpected challenges. Healthcare systems, and the people working in them, faced exceptional hardships being on the front lines to defend the world against COVID-19. They were also oftentimes overwhelmed by it. While there are many lessons still being learned from the pandemic, we are taking note of those pertaining to healthcare design. Specifically, we identified medical gas systems as being a critical component in combatting a pandemic. Their effectiveness in doing so often depends on the dialogue between building owners and engineers during design. Here, we will cover the most important topics you should discuss with your engineer during design.
Medical gas systems are critical to the life support, comfort, and wellbeing of the patients they serve. They also impact the efficacy of surgical teams and other caregivers.
Understanding Medical Gas Design and Its Importance
Medical gas systems are critical to the life support, comfort, and wellbeing of the patients they serve. They also impact the efficacy of surgical teams and other caregivers. Due to this, building codes that govern medical gas design and construction are very strict and clear about system requirements around safety measures, redundancies, system monitoring, and materials.
Medical gas systems begin with source equipment (i.e. pumps, compressors, and high-pressure cylinders) that generates or stores gases. As shown in the diagram below, these gases are delivered through a network of piping originating at the source equipment, travelling through the building across ceilings and up through floors, then ending at outlets in patient rooms, as well as surgical and support areas. Along the way to these outlets, the piping is outfitted with a series of valves for emergency shutdown along with pressure sensors and alarms to monitor gas flow and source equipment status.
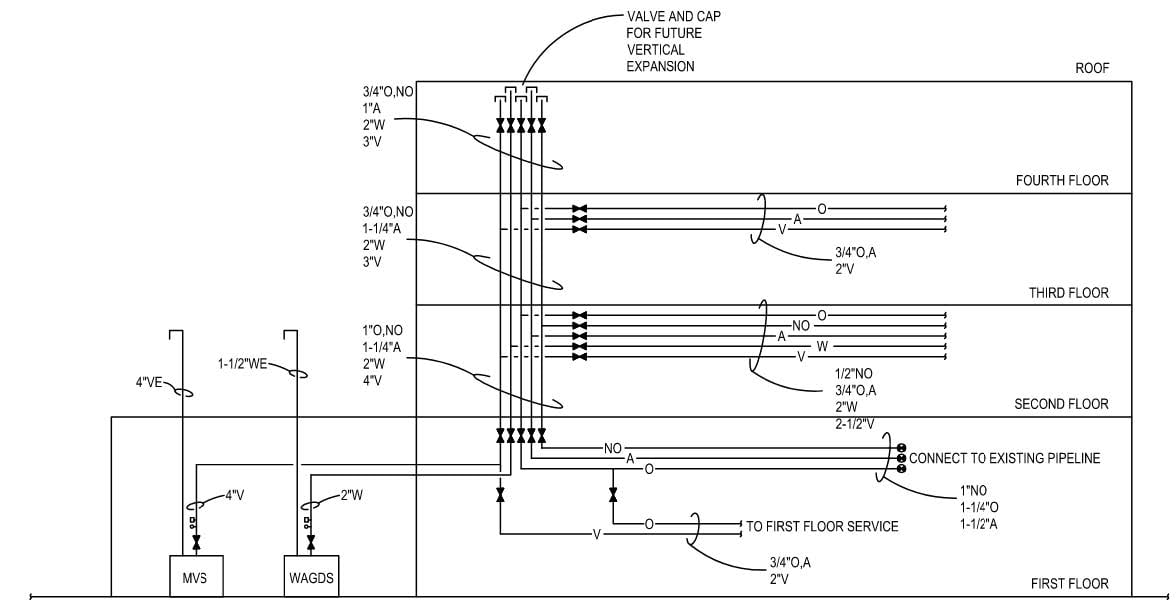
In addition to these safety measures, building codes require that source equipment be designed with some inherent redundancy or provisions for an emergency gas supply. For example, medical air plants must be sized for N+1 redundancy, meaning that if one compressor in the plant fails, there is at least one more of equal size to assume the lost system capacity. A system’s ability to deliver gas to a patient or a medical device depends on both the size of the source equipment and the size of the pipe conveying the gas. The size of the source equipment determines how quickly gas can be generated.
The size of the pipe determines how much gas can be delivered to the point of use. Engineers must consider both factors when designing a new system or renovating an existing one—if either is chosen incorrectly, the system may perform poorly or not at all. For example, a large medical air compressor may be sized to deliver air to a given number of COVID patients on ventilators, but if the piping is too small, it will naturally restrict the flow of air to them. Conversely, large piping may be able to deliver the needed volume of gas to patients, but a small compressor will not generate it fast enough.
Despite all the redundancies and safety measures in medical gas systems, the COVID-19 pandemic pushed many to their limits and often overwhelmed them. While building codes mandate these measures and are often meticulously inspected during construction, determining required system capacity is ultimately left to the design engineer with input from the owner. The infrequency of major pandemics did not trigger many health systems and engineers to plan for them. Thus, most medical gas systems simply were not designed to handle a respiratory virus outbreak.
Challenges Faced by Existing Medical Gas Systems
The life support function of medical gas systems is primarily provided by gases that support respiration, namely oxygen and medical air. Being that COVID-19 is a highly contagious respiratory disease, the added demand it put on oxygen and medical air systems was high and swift. Its fast spread also did not allow for much planning or reaction time.
The most severe cases of COVID-19 incapacitated the respiratory systems of those it attacked. People required ventilators for life support, and often for extended periods of time. As the number of COVID-19 cases surged, health systems were quickly pushed over capacity in terms of bed space, ventilators, and other support equipment. Stories of makeshift ICUs and COVID-19 wards, depleted oxygen supplies, ventilators operating in ways they were never intended to, plus difficult triage decisions were common. Many of these challenges can be traced back to a lack of foresight and preparation, especially in terms of medical gas system design.

The Reasons Behind the Challenges
Medical gas system design is largely driven by building codes, namely Chapter 5 of the National Fire Protection Association (NFPA) Code 99 – Health Care Facilities Code. This code establishes many of the safety and redundancy requirements mentioned earlier. However, one critical design element that it is largely silent on is system capacity. Capacity of medical gas systems are ultimately determined by the design engineer through consultation with the building owner and user groups, and informed by the design engineer’s experience and adherence to design guidelines that have no legal authority. Furthermore, the engineer must design to the scope and budget set by the owner. Therefore, unless the owner budgets for and directs the engineer to include provisions for battling pandemics, there will be little inherent system capacity to do so. Given the rarity of major pandemics, neither building owners nor engineers had much perspective on the importance of preparing for them before the COVID-19 outbreak.
Along with little spare capacity, medical gas systems were quickly overwhelmed because ventilators were needed to support the most severe COVID-19 cases. Ventilators represent one of the largest loads that can be placed on oxygen and medical air systems—some ventilator types consume over 10 times as much gas as normal breathing. Therefore, as COVID-19 cases increased and more ventilators were added to treat them, systems never designed to handle them were quickly depleted. Medical gas suppliers similarly lacked the infrastructure to replenish these systems, as the demand was unlike anything they had experienced.
Ventilators represent one of the largest loads that can be placed on oxygen and medical air systems—some ventilator types consume over 10 times as much gas as normal breathing.
With medical gases in short supply and health systems overwhelmed with new cases, the desperation to save lives by any means possible may also have amplified system capacity issues. As treatment resources and options became scarce, caregivers often resorted to any solution available to them, even if it was not the most correct one (BeaconMedaes USA [BM], 2020). Stories of connecting multiple ventilators on a single gas outlet, placing multiple patients on a single ventilator, and other risky acts were common. Extreme actions like these often placed equally extreme demands on medical gas systems (BM, 2020).
What We've Learned (So Far)
While we are still learning many lessons on dealing with pandemics, some are already clear. The first and perhaps most important lesson is that successfully combatting a pandemic requires effective planning, forethought, and execution. As mentioned, a lack of all these things resulted in medical gas systems having little capacity for the stresses of COVID-19, but those designing, maintaining, and operating them were also unprepared. As health systems were pushed beyond their ability to treat new COVID-19 cases, they sought solutions from engineers and other design professionals who were working reactively to find them (BM, 2020).
Medical gas system engineers were often left scrambling to find ways to build additional capacity into existing systems. The primary challenge in finding solutions to this was that many engineers had little to no experience to draw upon. Once they have a clear design scope from the building owner, engineers determine the needed capacity of a medical gas system from empirical data collected over many years. However, this data represented usage during relatively normal times and not extreme cases like a global outbreak of a respiratory disease. The onset of the pandemic prompted thought leaders in medical gas design to publish guidelines and strategies to respond to it based on the best information they had (BM, 2020). Now, with the pandemic beginning to ease, more research around this topic is becoming available. Design guidelines are also being further reviewed and refined.
Another early lesson from COVID-19 is that pandemic response planning needs to be an integrative and collaborative process. Input from a variety of experts is needed to craft and execute these plans. Pulmonologists, infection control specialists, nurses and other front-line caregivers, hospital administrators, building facility managers, medical equipment manufacturers, and building design professionals should all be included in the planning process. Design professionals will need detailed information about how the medical gas systems and built environment will be integrated into response plans.
Facing the Challenges
Developing a pandemic response plan is obviously a monumental task and designing medical gas systems appropriately is only one aspect of executing it. However, given what we have already learned over the last 15 months coupled with prior experience, engineers are becoming more conscious of how to approach this challenge. While knowledgeable engineers will know what questions to ask their clients, it is valuable for all parties involved in pandemic response to be aware of what information will be needed. While we have seen calls from our clients for “pandemic-ready” facilities, there are many different ideas of what pandemic readiness entails. Coming to agreement on details of this early in design is paramount.

Pandemic response plans should be clear on where and how these patients will be treated and then have treatment areas designed with provisions to accommodate them.
Many facilities that treated severe COVID-19 cases were overwhelmed by their volume and found themselves treating COVID-19 patients in spaces never designed for it. Pandemic response plans should be clear on where and how these patients will be treated and then have treatment areas designed with provisions to accommodate them. Engineers and other design professionals will need to know where these spaces will be located and realistic estimates of how many pandemic patients will be treated in them. Plans should also consider spaces that will have a dual function between their primary use and pandemic treatment. For example, observation areas in ERs are often used for triage in mass casualty events, but the former function has a much lower medical gas demand and requires less system infrastructure than the latter. When navigating dual-function spaces, engineers will generally design medical gas systems for the worst-case scenario.
Design professionals will also need details about how pandemic patients will be treated and with what medical devices. Healthcare professionals may have to educate them on this, especially in cases of newly discovered diseases. For instance, most engineers were aware that severe COVID-19 cases required ventilators for treatment, but fewer knew what types of ventilators to design for. Ventilators have a wide range of gas consumption depending on type—standard invasive types use around 12 liters per minute while non-invasive high flow types use up to 50 liters—and this can introduce a high level of variability in system sizing (BM, 2020). Other treatment devices (e.g., nasal cannula, reservoir masks, etc.) may have similar variations on consumption, and thus specifics on them should be given to the design team as early as possible. Engineers can make gas consumption estimates based on equipment type, but they will look to eliminate uncertainty and risk wherever possible, especially where an assumption could yield highly variable results. Providing equipment manufacturer literature removes ambiguity and better ensures good system performance.

Construction budgets also have a role in how medical gas systems are designed and building owners may have to make difficult choices in how robust they are. Engineers fortunately have some cost-saving measures at their disposal where this is concerned. As mentioned earlier, a system’s ability to deliver medical gas depends on the size of both the source equipment and the delivery piping. Piping must be adequately sized for pandemic response at the time of construction to avoid costly renovations later, but source equipment does not necessarily need to be.
A surge in gas consumption can be met by adding new or expanding existing source equipment when the surge occurs. This is often a better approach from a cost and system performance standpoint. For example, medical air plants can be sized to accommodate normal demands, but outfitted with the ability to quickly add additional compressors during surges. If a building owner prefers to size the plant for a pandemic immediately, the compressors can be equipped with variable speed drives for energy savings. Designing oxygen source equipment for surges tends to be more complicated, especially with cryogenic systems (i.e., bulk liquid tanks and smaller dewar containers). Liquid oxygen in these tanks naturally evaporates over time and is expelled as waste. The amount wasted increases during periods of low demand and thus equipment sized for the demands of a pandemic will waste more oxygen during normal use. Therefore, it is more cost effective to design for expansion or addition of source equipment, such as creating a connection point for an emergency oxygen supply, like a high-pressure cylinder manifold, to be added later.
While the previous design considerations are important for both new construction and renovation projects, the latter presents its own set of challenges. The ability to renovate systems in existing healthcare facilities may be constrained by availability of space for new source equipment, sizes of existing piping, ability to bring systems up to current codes, tolerance for disruption to active treatment areas, and cost implications.
To navigate these challenges, engineers often need a thorough understanding of existing systems before determining the best approach for redesigning them. Intensive surveys of these systems, conducted by both engineers and building facilities staff, are immensely helpful. As healthcare facilities tend to be remodeled often, keeping accurate records of what and when changes occurred can minimize the risk of design errors and increased construction costs. Engineers will want to review all construction drawings of existing systems, along with details of past renovations and issues, and will design from the best information made available to them.

ERDMAN Takeaway
While we have discussed some of the lessons learned about medical gas design for pandemics, there is undoubtedly more to learn. As more information becomes available, our design professionals will be reviewing it and developing best practices for battling pandemics. Meanwhile, we encourage our clients to do the same. Awareness of other highly infectious diseases, how to treat them, and the likelihood of an outbreak is key in designing for the future.
Designing for pandemic readiness, particularly in medical gas systems, needs to be a collaborative effort among those who design them, as well as those who use and maintain them. Successful medical gas design is not limited to engineers—it is a combined effort among engineers who size the systems, architects who integrate them into the built environment, caregivers who provide feedback on how they will use them, and facility staff who maintains them. All these parties need to be involved in making decisions that shape how pandemic treatment is administered.
Whether or not your facility was on the front lines of the battle against COVID-19, we recommend assessing readiness for a future pandemic. You should then use this assessment to determine if any building upgrades would be helpful in treating future diseases or reducing the risk of spreading them. Our design and construction professionals can assist with this effort and offer services ranging from facility assessments to physical remodels of existing spaces and systems.
- BeaconMedaes USA. (2020, April). Sizing Medical Gases for COVID 19. https://acprodbponlinebcc5.blob.core.windows.net/bp-public-files/bp_editor_div_mgs/SalesMarketing/Bmed_Paper_Covid_Sizing_HTM_EN.pdf



