Given the pandemic’s acceleration of certain healthcare trends, health systems will require more focused strategic planning on several fronts utilizing sophisticated data analysis.
The pandemic accelerated several trends that indicate a waning reliance on traditional healthcare delivery systems. These trends include care delivery alignment with regulations focused on prevention and cost containment, increased access to ambulatory care, home and community-based services, and technological innovation that deepens the shift in care to the outpatient setting or out of a clinical setting entirely (e.g. telehealth). COVID surges strained resources on the acute care platform, resulting in lost revenue and delayed care. Meanwhile, procedural and diagnostic platforms sat idle. Many of those who suffered from the virus continue to experience a wide variety of ailments ranging from anxiety, depression, and psychosis to heart, lung, and inflammation issues. Many patients will even require long-term management of COVID symptoms. Much of this monitoring and care will indeed take place outside traditional models.

As health systems continue to respond to variant strains, the pandemic emboldened nontraditional players to enter or strengthen their market positions. Non-hospital owners, focused on coordinated and cost-conscious care (such as large payors), now own a substantial portion of all ambulatory assets. The decline in individual lives covered by employer-sponsored plans creates more leverage for government backed and exchange plans to influence future commercial offerings. Since there is more awareness of how social determinants influence overall health, new types of coverage may expand into areas not typically pursued by commercial payors.
Acceleration of these trends will require the leadership of health systems and hospitals to double down on their facility and access strategies to respond to change. The traditional approach to master planning, in which forecasted facility demands consider changing utilization rates, ceases to be reliable. A switch to home-based and digital care demands the same attention as growth and shifts inside the acute care and ambulatory clinical platforms. Additionally, as Medicare reimbursement is now more closely tied to patients’ satisfaction with their overall care experiences, providers are incented to improve quality of care. Competition is no longer just the health system down the street — it is a less structured, consumer- and employer-driven environment increasingly influenced by ambulatory, chronic, and post-acute care delivery. Health systems must remain nimble and flexible to effectively compete with more sophisticated players while continuing to address the local community’s health needs entering this post-COVID environment. Finally, interoperability and advancing health technology such as Apple Watches, ECG monitors, biosensors, and other wearables will continue to disrupt the way consumers track their health and receive care.
Four Emerging Trends Reshaping Hospitals
As we consider the current environment as part of the post-pandemic recovery, there are four trends that will reshape how hospitals emerge from COVID-19:
1. An acceleration in the move from inpatient to outpatient
The Kaiser Family Foundation (n.d.) reports that overall, inpatient days declined by 0.1% annually, from 566 to 564 days per 1,000 population while outpatient visits increased by 1.5% annually, from 2,250 to 2,392 per 1,000 population between 2015 and 2019.
The Advisory Board estimates that the overall proportion of inpatient medical days will increase from approximately 71.1% to 72.3% of all inpatient days between 2020 and 2030, respectively. This indicates a shift in surgeries to the outpatient setting (Woodrow & Gelbaugh, 2021). Several issues caused this shift, including technological advancements, consumer demand, and payor pressure (Kumar & Parthasarathy, 2020).
Inpatient Days Trending - Medical and Surgery Groupings
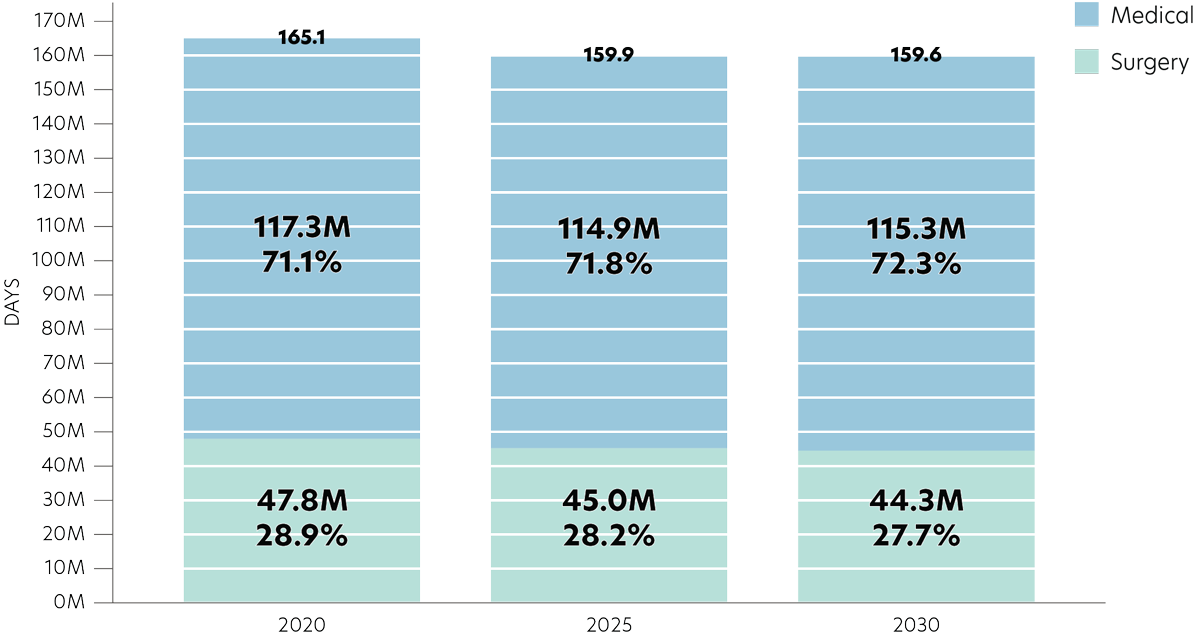
Source: the bar chart data is from Advisory Board.
2. A shift to managed care and alternative payments
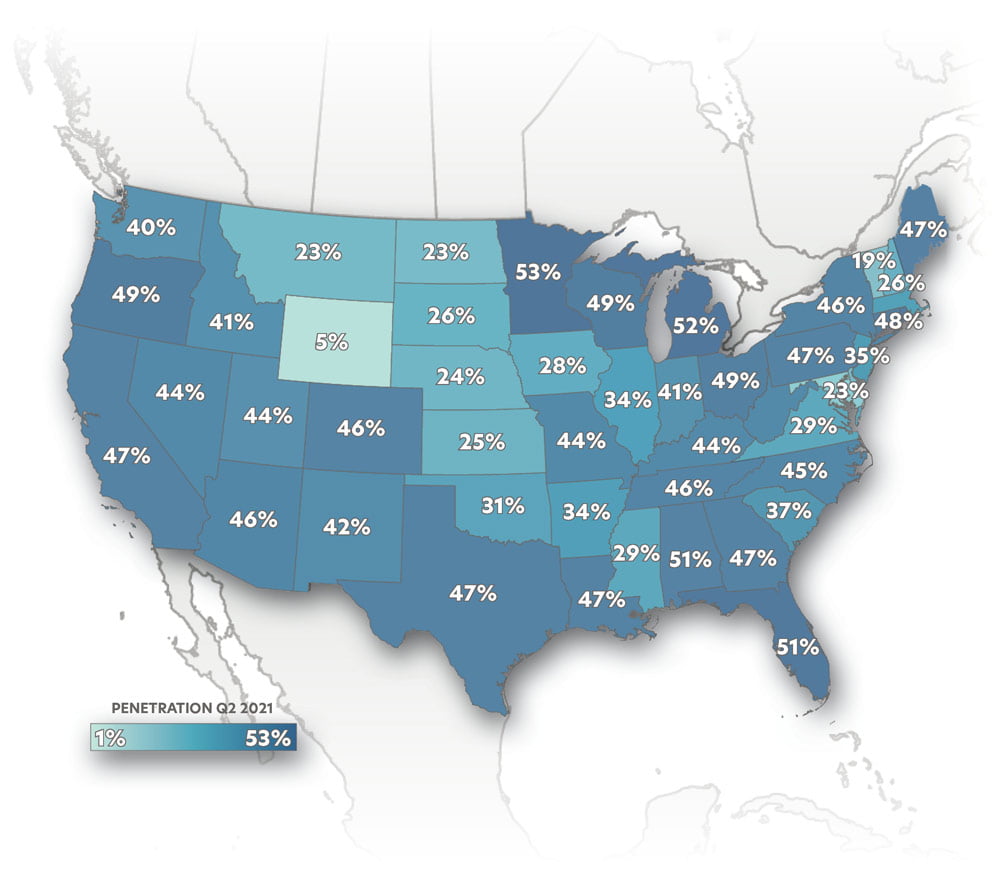
The percentage of Medicare Advantage patients among those eligible for Medicare increased by six percentage points between the end of 2017 and 2020 (overall 34% vs. 40%), but increased three percentage points in the first six months of 2021 alone (overall 40% vs. 43%) (Center for Medicare & Medicaid Services, 2021). In all, penetration in 42 states increased faster during this time. Similarly, 34 states showed higher increases in dual-eligible members in the six months ending with June 2020 than the average annual increase between 2016 and 2019 (Center for Medicare & Medicaid Services, 2021).
MEDICARE ADVANTAGE PENETRATION
QUARTER 2 OF 2021
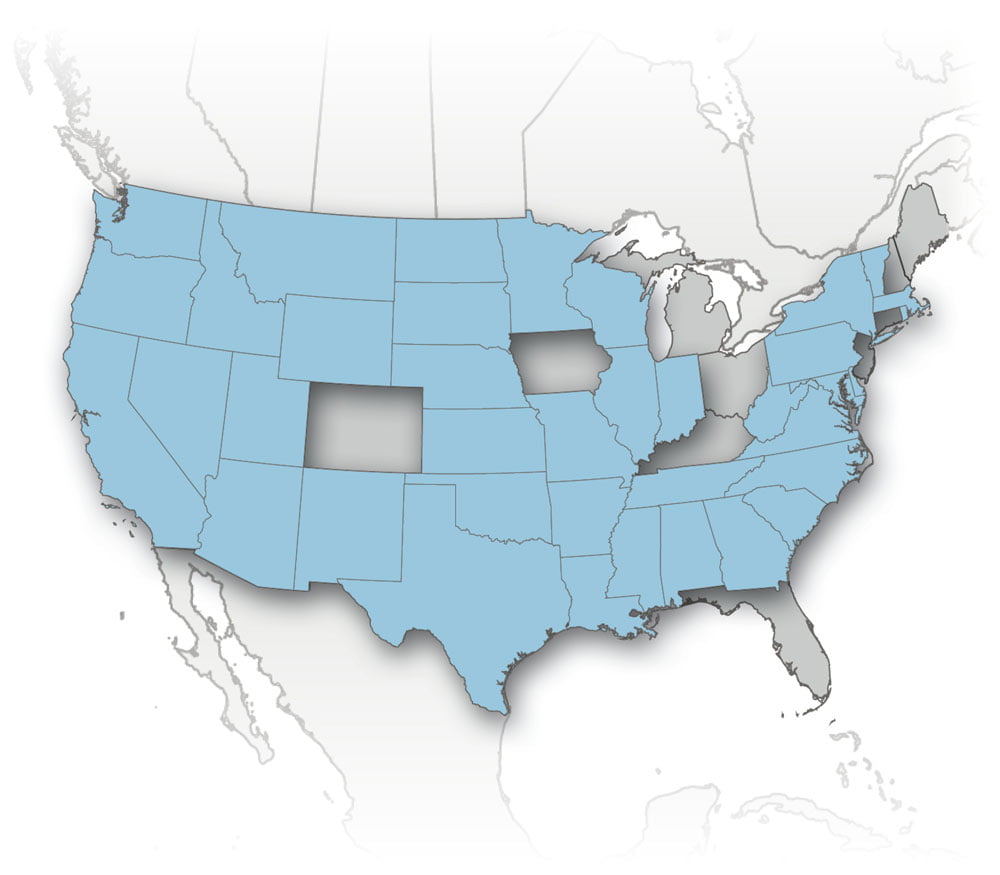
STATES IN WHICH INCREASE IS FASTER IN 6 MONTHS THAN BETWEEN 2017-2021
3. Increased accessibility through digital and home-based solutions
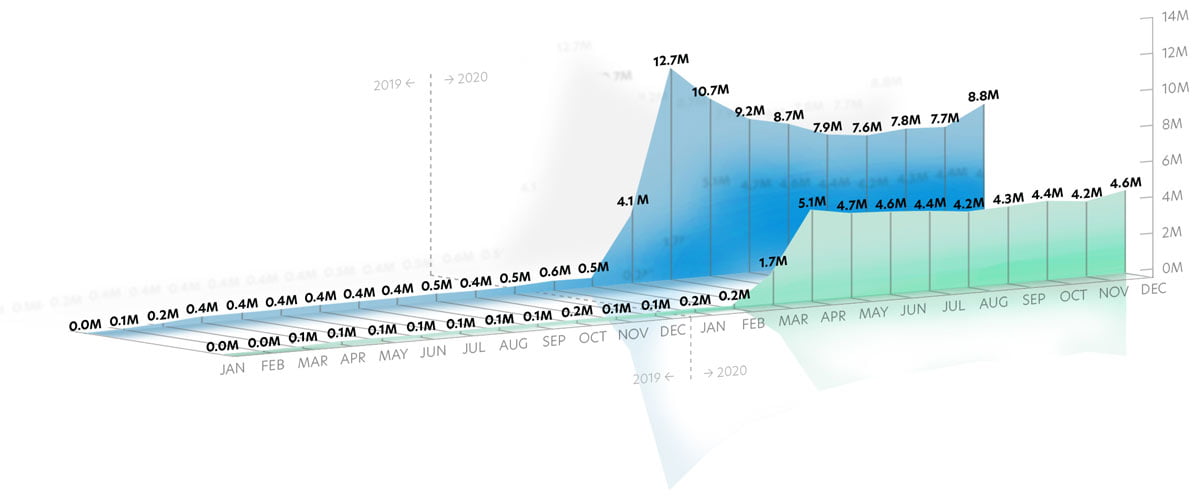
The pandemic saw a substantial and necessary increase in telehealth visits as hospitals and other facilities closed. A recent Mayo Clinic and MITRE Corporation study showed that telehealth visits increased between 10- and 100-times prior volumes in most states between February and April of 2020, followed by a gradual decline. However, between September and December of 2020, telehealth visits with primary clinical classifications such as respiratory, infectious and parasitic diseases, neoplasms, musculoskeletal and connective, circulatory, nervous and sensory organs, endocrine, and digestive systems rebounded by an average growth of approximately 21% (COVID-19 | Healthcare Coalition, 2021).
While states have seen a drop-off in telehealth visits, many health care providers will continue to utilize this technology — especially as it relates to mental health conditions. For example, in April of this year, mental health conditions accounted for approximately 58% of telehealth visits by diagnosis (Fair Health, 2021). According to Sg2 (2021), by 2030, up to 30% of ambulatory visits could be telehealth visits, with many of these in behavioral health and as a complement to traditional office utilization in other medical and even surgical specialties, such as for post-surgical follow up visits.
By 2030, up to 30% of ambulatory visits could be telehealth visits.
NATIONAL TELEHEALTH CLAIMS
JANUARY 2019 THROUGH DECEMBER 2020
4. Impact of nontraditional players in the healthcare marketplace
Bain and Company (2021) reports that while M&A activity in the healthcare sector decreased in 2020, the percent of deals of less than $5 billion in total value increased from about half to more than 80% of the total value of all deals in 2020 compared to 2019. These smaller deals tend to favor private equity in smaller organizations such as physician groups.
Retailers such as Walmart and CVS Health are already delivering expedited, convenient, and integrated care at their walk-in and urgent care clinics. CVS specifically intends to scale up the number of HealthHUB/MinuteClinics to 1,500 locations by the end of this year (Paavola, 2019). Amazon Care also has approached large insurers to align with employer plans and provide primary care, telehealth, and other nontraditional services such as fitness through Precor’s Peloton. Its expansion is not limited to large employers or metropolitan areas; it is also targeting rural populations (Paavola, 2021).
Health systems aligned with payors offering value-oriented plans, or owning these plans themselves, may be more sustainable in a post-COVID environment. For example, McKinsey & Company reports that between 2016 and 2020, Medicare Advantage enrollees saw a 32% average reduction in premiums, and in 2020, 93% of those enrolled had access to a zero-premium plan. Additionally, these plans have improved outcomes over time, faster than commercially covered lives (Singhal, 2020).
Post-COVID, as the number of patients with chronic conditions increases, managed care plans that provide holistic benefits in fitness, nutrition, counseling, and fulfill social needs will increase.
Strategic Planning Requires Attention in Six Areas
Now that we’ve identified key trends driving how health systems will emerge from the pandemic, your strategic planning efforts require attention in six key areas:
- Reducing operating costs in inpatient, outpatient, and physician services to optimize contracting leverage: the increasing penalty for lack of price transparency may yet improve the incentive to focus on relationships
- Optimizing scope and access to primary and preventive health services to focus on whole-person care: this includes taking an active role in ensuring not only health and wellbeing, but also:
- Behavioral and psychological health
- Management of prescription drugs along with over-the-counter medications
- Nutrition as medicine
- Integrating digital connectivity across all domains of care management, such as care at home, post-acute transitions, and for customer relationship management
- Rationalizing capital and operating resources in the inpatient portfolio to optimize access, care coordination, payor contracts, patient access, volume, outcomes, and reputation
- Modernizing the master facility plan to optimize “bricks and clicks” access, competitive positioning, market growth opportunities, and efficiency
- Equipping leadership and governance to optimize monitoring and dynamic, strategic responses to changing market conditions
ERDMAN Takeaway
Given the pandemic’s acceleration of certain healthcare trends, health systems will require more focused strategic planning on several fronts utilizing sophisticated data analysis. To best address this, you will want to leverage the right resources. In our case, we offer ERDMAN Analytics. It represents an array of proprietary tools to help define target markets against industry data and insights. Findings can uncover regional consumers that best align with your healthcare offerings, in turn helping drive strategic decisions to plan for your facility needs. Considering the value that data analysis can offer as part of a strategic assessment, health systems can take effective action focused on key areas, ranging from reducing operating costs to equipping healthcare leaders with the information needed to respond to changing market conditions. Feel free to also connect with us today at info@erdman.com to start taking steps to optimize your healthcare strategy in the post-pandemic era.
What is ZeroIn™ by ERDMAN Analytics?
Center for Medicare & Medicaid Services. (2021, July). MMCO Statistical & Analytic Reports. https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/Analytics
Center for Medicare & Medicaid Services. (2021, July). Monthly MA Enrollment by State/County/Contract. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MCRAdvPartDEnrolData/Monthly-MA-Enrollment-by-State-County-Contract
COVID-19 | Healthcare Coalition. (2021, May). COVID-19 Telehealth Impact Study. https://c19hcc.org/telehealth/impact-home/
Fair Health. (2021, April). Monthly Telehealth Regional Tracker. https://www.fairhealth.org/states-by-the-numbers/telehealth
Haxer, J. et al. (2021, March 16). Healthcare M&A: A Pandemic-Induced Slowdown in Every Sector. Bain & Company. https://www.bain.com/insights/m-a-global-healthcare-private-equity-and-ma-report-2021/
Kaiser Family Foundation. (n.d.). Providers & Service Use. https://www.kff.org/state-category/providers-service-use/
Kumar, P., & Parthasarathy, R. (2020, September 18). Walking out of the hospital: The continued rise of ambulatory care and how to take advantage of it. McKinsey & Company. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/walking-out-of-the-hospital-the-continued-rise-of-ambulatory-care-and-how-to-take-advantage-of-it
McDowell, M. (2021, June 3). Sg2 2021 Impact of Change® Forecast: Post-Pandemic Recovery, Rising Acuity and Ambulatory Shifts. https://www.sg2.com/health-care-intelligence-blog/2021/06/sg2-2021-impact-of-change-forecast/
Paavola, A. (2021, July 7). Amazon Care approached big health insurers to expand coverage. Becker’s Hospital Review. https://www.beckershospitalreview.com/strategy/amazon-care-approached-big-health-insurers-to-expand-coverage.html
Paavola, A. (2019, June 4). CVS to open 1,500 HealthHub stores by the end of 2021. Becker’s Hospital Review. https://www.beckershospitalreview.com/pharmacy/cvs-to-open-1-500-healthhub-stores-by-the-end-of-2021.html
Singhal, S. (2020, September 9). The great acceleration in healthcare: Six trends to heed. McKinsey & Company. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/the-great-acceleration-in-healthcare-six-trends-to-heed
Woodrow, L., & Gelbaugh, C. (2021, July 23). Q&A: What strategic planners need to know for 2021. The Advisory Board. https://new.advisory.com/blog/2021/07/strategic-planner-survey



