Last week, the Centers for Medicare and Medicaid Services (CMS) released results for healthcare spending for 2018:
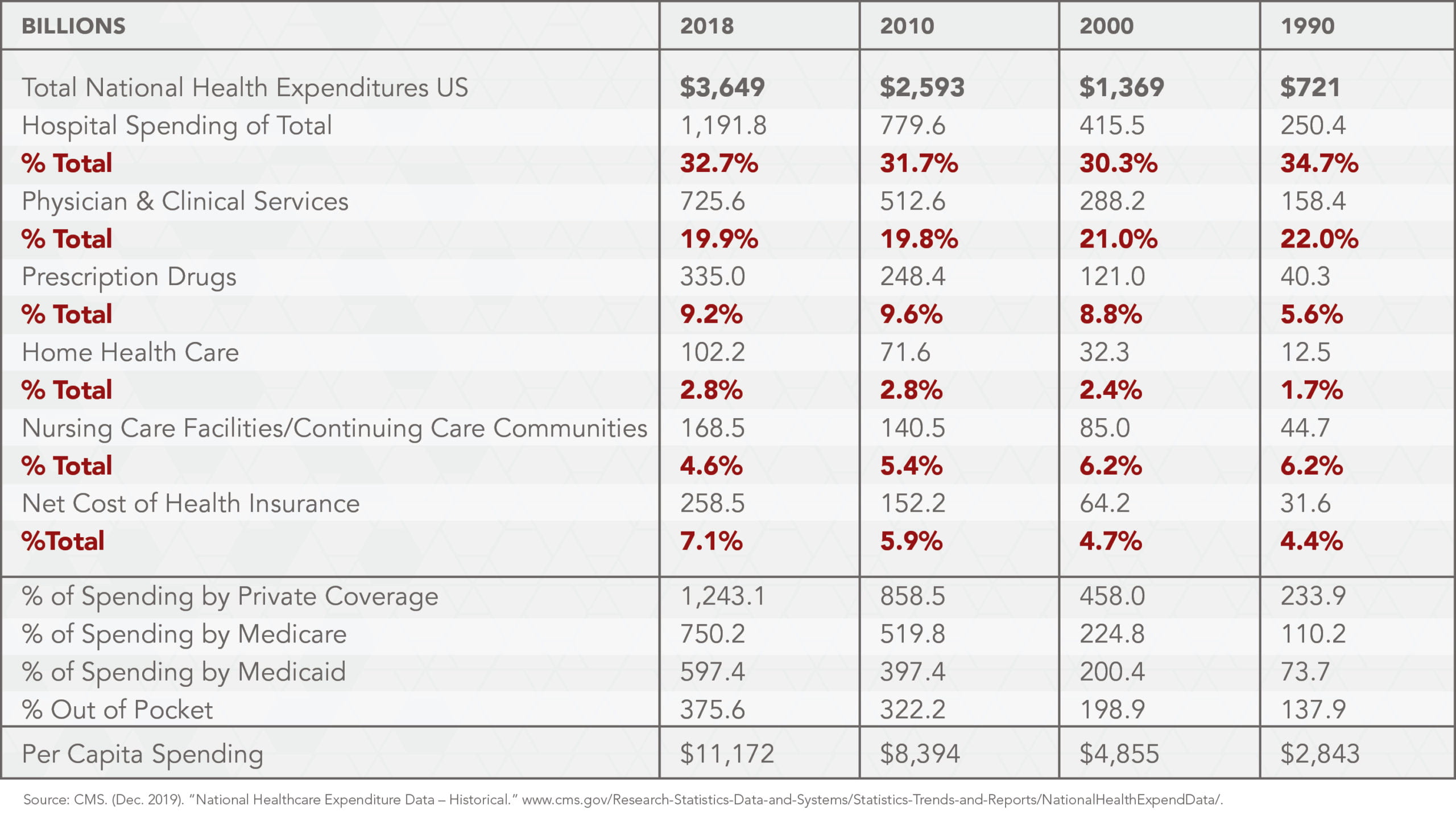
“U.S. health care spending increased 4.6% to reach $3.6 trillion, or $11,172 per person in 2018. The growth in 2018 was faster than in 2017 when health care spending increased 4.2%. The faster growth in 2018 was associated with faster growth in the net cost of health insurance, which increased 13.2% following growth of 4.3% in 2017, due primarily to the reinstatement of the health insurance tax in 2018. The overall share of gross domestic product (GDP) related to health care spending was 17.7% in 2018, down from 17.9%in 2017. The insured share of the population was 90.6% in 2018 and 90.8% in 2017, as the number of uninsured increased by 1 million to 30.7 million in 2018.”
Hospital Price Transparency
That healthcare spending is increasing faster than the country’s gross domestic product and overall inflation rate is not a surprise: it’s a trend that has continued for 60 years. For instance, it was 5% of GDP in 1960, 12.1% in 1990 and 17.7% today with no end in sight.
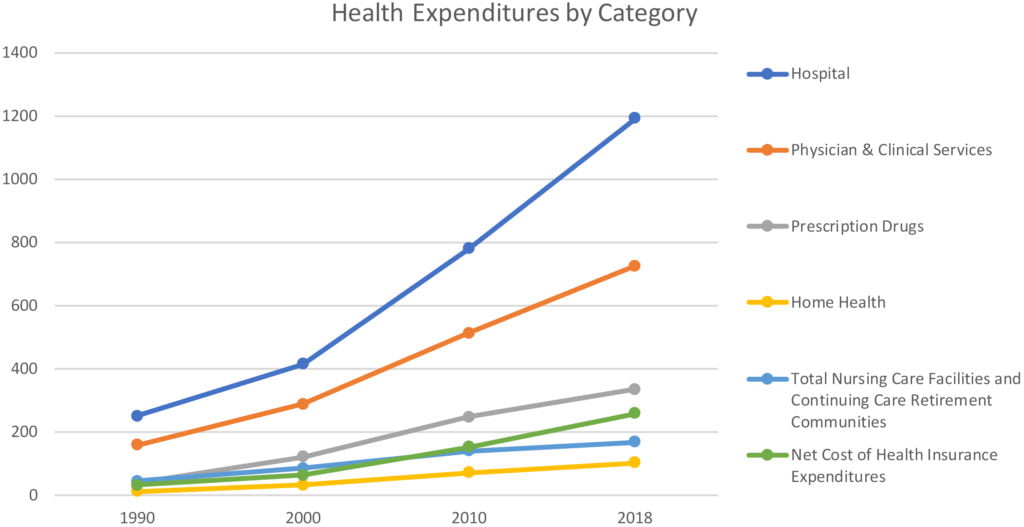
What’s surprising are the changes in where health dollars have been spent: hospitals and physicians have held their own, insurers have fared better, and nursing homes have lost ground.
In the 28-year period reflected below, the senior population has grown while demand for acute beds has shrunk. Access to physician specialists has remained adequate especially in urban communities but shortages of primary care and specialists in rural settings is problematic. Older, sicker people are being treated outside hospitals in outpatient clinics and medical offices, in nursing care facilities, and at home but nursing homes/continuing care communities have lost ground to other sectors in maintaining a proportionate share of spending.
These numbers illustrate the enormity and complexity of the healthcare industry—labor intense, technology-dependent, high profile and competitive. Like other industries, it is adapting to big changes in our society that have evolved over the past 50 years:
- Urbanization of the population with diverse ethnic, political, and social experiences and expectations
- Workforce diversity and shift from manufacturing to offices and homes
- Aging of the population in tandem with growing income inequality
- Technology-driven disruption in key industries like transportation, financial services, media, education, healthcare, etc.
- Generational shift away from institutional loyalties and trust
While demand for acute care has declined over the past 28 years, hospital spending has increased by more than 375%. Use of home health does not appear to have quelled hospital price increases, nor have advancements in prescription drugs. Spending data suggests these advancements have been cost-added benefits to the system rather than cost reducing.
Unlike other industries, the health care industry’s economic growth seems uncontrollable to policymakers, insurers, employers, and consumers who think it’s out of control. Granted, its challenges are unique (below). But they’re not insurmountable:
- Acceleration of therapeutic innovations that deliver evidence-based care, personalized care to patients but with hefty prices
- Increased accessibility of capital from private investors and banks to fund facilities and programs sponsored by stronger organizations
- Intensified tension between insurers and providers seeking to access patients (consumers) and control predictable revenues
- Increased competition for talent
- Increased pressure on operating costs for labor, supplies, technologies, facilities
- Increased regulatory risks as the scale and scope of operations extends beyond traditional acute and ancillary businesses
- Decreased demand for inpatient services and increased complexity of those hospitalized
- Increased dependence on health information technologies in workflow optimization interoperability, privacy, security, affordability and user experiences
- Increased pressure from physicians to address their Issues of compensation, burnout and operational frustration
- Increased importance of advocacy efforts to influence policies and laws at local, state and federal levels
- Increased competition from privately-funded niche players targeting profitable hospital and medical group services
- Increased impact of large vertically integrated health systems that combine insurance, retail health and primary care services
- Increased pressure from insurers and medicare to implement value-based purchasing programs
- Increased workforce dissatisfaction
- Increased transparency about prices, business relationships and quality.
- Increased competition for C suite talent
- Increased pressure on boards to be effective in their fiduciary role
- Declining public trust in the U.S. health system
Efforts to cut operating costs in the workforce and supply chain are standard operating procedure. Improvements in business office administration, cash flow management and reimbursement, strategic partnerships, and consolidation are on the board agenda in each. But that’s not enough.
Success by hospitals, physicians and senior living providers is dependent on bold, visionary actions to compete based on differentiation by convenience, cost and user experiences. That means physical facilities that are convenient and digitally connected to homes and workplaces. That means services that are available virtually 24/7 and care teams that interact skillfully. That means a willingness by boards and managers to create a future that’s respectful of tradition but not paralyzed by sacred cows.



