Abstract
Market forces are driving significant changes to the way hospitals operate in their communities. Clinical innovations are shifting sites for care from inpatient to outpatient and home settings. Insurers, Medicare and Medicaid are shrinking their reimbursement. Consumers are demanding modern facilities, digital connectivity, lower costs and improved convenience. Competition is intensifying between traditional hospital competitors and new limited-service facilities funded by private investors. This is the environment in which hospitals now compete.
Micro-hospitals offer community hospitals and health systems a strategy to respond to these market forces. There are more than 60 micro-hospitals currently in operation. Most were developed by or in partnership with local health systems or private investors within the past five years. Micro-hospitals serve low-acuity patient populations requiring minimal inpatient, outpatient, diagnostic and emergency services. They are located, designed and built as a strategic element of a health system’s deployment plans or as an attractive use of capital.
Micro-hospitals, if designed appropriately, accrue four strategic advantages to hospital sponsors: broaden market expansion, lessen capital risks, decrease operating costs and increase consumer appeal. They are designed and built to optimize patient experiences, maximize staff productivity and serve as a flexible footprint for additional services as demand warrants. While the regulatory climate for micro-hospitals is volatile, the sector is expected to grow as health systems deploy capital to micro-hospital projects. Therefore, micro-hospitals serve as a critical element of a hospital’s strategic plan for growth and scale.
Micro-hospitals are emerging as a distinct sector that offers an array of acute, ancillary and retail services, while offering a lower-cost alternative to traditional hospital-outpatient facilities
Background: Micro-Hospitals
Micro-hospitals have been around since 2007 and currently operate in 19 states. Sometimes called “neighborhood hospitals” or “mini-hospitals,” they range from eight to 30 beds, in facilities ranging from 15,000 to 60,000 square feet. Consultants estimate 60 micro-hospitals have been built in the past five years with another 40 new projects coming online in the next two to three years. The majority of these are sponsored by local health systems as a key element of their deployment plans.

While there is no prototype for micro-hospitals, they typically serve medical and surgical patient populations at low risk, entailing shorter stays and lower costs per admission. Micro-hospital capabilities also include labs, imaging, outpatient surgery, pharmacy, primary and preventive health and emergency care for non-life-threatening conditions. Additionally, many sponsors develop medical offices, outpatient physical therapy, health education and common areas for community use.
Federal regulation governing micro-hospitals has focused primarily on their eligibility for Medicare reimbursement (Medicare Conditions of Participation). Per the Centers for Medicare and Medicaid Services, a micro-hospital must be primarily engaged in inpatient care and have at least two inpatients at the time of their accreditation visit. State by state, requirements vary, and may also have requirements relating to inpatient services.
Two Strategies Emerging in Micro-Hospital Development
Development of micro-hospitals is being led by health systems and independent investors/sponsors with different aims:
DEVELOPER | LOCAL HOSPITAL / HEALTH SYSTEM | INDEPENDENT SPONSOR |
|---|---|---|
PRIMARY OBJECTIVE | Enhance the hospital’s access and patient capture in targeted communities as an element of a deployment and strategic plan. Serve as a footprint for subsequent expansion of the hospital’s services in neighboring communities. | Achieve a favorable return on capital through referrals from physicians, patient preference, and network inclusion by insurers.
Many anticipate partnerships with health systems. |
POSITIONING
STRATEGY | An independent, state-of-the-art facility offering primary and secondary services that are safe, effective, easily accessible and efficiently operated. A convenient, cost-effective alternative to traditional hospital services that optimizes patient experiences. Lower operating costs are achieved through streamlined operations and independence from local hospital overhead. | A state-of-the-art facility offering primary and secondary services that are safe, effective, easily accessible and efficiently operated, and backed by a reputable, full-service hospital. A convenient, affordable source of healthcare services connected to a reputable health system offering convenient clinical capabilities and support services. Maintenance of low cost operating model to optimize negotiations with payers. Smaller, more consumer-friendly scale for environment of care. |
KEY RISK FACTORS | Regulatory compliance with state and federal agencies in relation to access, safety, outcomes, and patient experiences. | Regulatory compliance with state and federal agencies in relation to access, safety, outcomes, patient experiences and ownership interests, including back-up safety obligations. |
Inaccurate assessment of market demand and opportunity. Failure to build suitably for expanded scale and scope of services (flexible design). Ongoing support by the local medical community. | ||
KEY CLINICAL CONSIDERATIONS | Connectivity to and coordination with clinical programs in the hospital to ensure continuity of care, safety, quality and risk management. | Connectivity to upstream providers for services not provided (network design) via contractual relationships. |
Clinical protocols for each designated inpatient, outpatient and diagnostic programs. Clinical innovations in technologies and care management techniques that require facility and operational adjustments to achieve certification/accreditation. Staffing by clinicians, nurses, technical support and ancillary staff (care team coordination around targeted patient populations). | ||
KEY OPERATIONAL CONSIDERATIONS | Patient Capture: Referral relationships with physicians, preferential inclusion in insurer networks, and retail/direct-to-consumer services and programs offered in a modern, convenient facility | |
Clinical Assessment: Analytics, diagnostic testing protocols,
risk stratification. In most, patient information is entered into a
personalized medical record attached to attending physicians
and other services used in the health system. | Clinical Assessment: Analytics, diagnostic testing protocols,
risk stratification. | |
Care Management: Evidence-based protocols, clinical process improvement, team-based care design, outcome measurement, formulary design & medication management, patient education, discharge planning, nutrition (food services). | ||
Administrative Services: Compliance monitoring & reporting, marketing, facility maintenance, digital health connectivity, payer contracting, physician relations, patient satisfaction monitoring | ||
CRITICAL SUCCESS FACTORS | Location Selection: Acquiring a location that’s accessible to targeted populations, conducive to future growth, and near necessary hospital support services. Near related health services, clinicians and facilities. Intelligent Facility Design: Flexible design to accommodate addition of services and capabilities AND operational efficiency that supports favorable cost positioning with payers. | |
Patient Experience: Personalization of services that optimize convenience, connectivity, cost effectiveness, patient experiences and affinity for the sponsoring health system. | Patient Experience: Management that optimizes convenience,
connectivity, cost effectiveness, and patient experiences. | |
Integration in the health system’s long-term growth strategy. | Favorable competitive positioning via cost, access, facility
design and capabilities compared to local hospital services. | |
Physician, allied health and nursing capabilities, accessibility, and team orientation | ||
Clearly, the rationale for developing micro-hospitals varies depending on the strategic aims of the sponsor. Return on capital goals is different if a micro-hospital is part of a health system’s long-term master site plan for growth and a private investor’s goal is profitability. Both must remain flexible in the scale and scope of services offered as market opportunities evolve, regulations emerge, licensing and accreditation standards are codified, consumer expectations change and competition heats up. Thus, for a community hospital or health system sponsor, the investment in a micro-hospital is both an offensive and defensive strategy: to strengthen competitive positioning and protect against competitive encroachment.

The ERDMAN Perspective: Planning for Micro-Hospitals
The objectives for development of a micro-hospital depend on the sponsor’s aims. Optimal return on capital and reputation are the result of careful planning and meticulous execution. Physical facilities, staffing, workflow, patient interactions, and the range of ancillary services must be anticipated in the context of a micro-hospital: it is not a small hospital, it is a hybrid requiring intelligent design premised on a vision for care delivery in a unique setting. A successful micro-hospital should not be built through the lens of a traditional hospital facility plan.
Assessing the market opportunity for a micro-hospital involves a three-step process prior to breaking ground:
- Market Opportunity Analysis (MOA): Analytics that quantify the optimal clinical program opportunities based on anticipated demand and utilization, reimbursement considerations, state and federal regulatory constraints and expectations from insurers, physicians, employers and the public are vital. ERDMAN’s Micro-Hospital MOA Model™ provides data necessary to defining and timing the scale, scope and capital required for a successful micro-hospital development that is complementary to the sponsor’s strategic aims.
- Strategic Planning: Sponsors of a micro-hospital must determine its short- and long-term capacity requirements in the context of broader mission and competitive considerations. A micro-hospital might evolve to a hub for a wide array of inpatient, outpatient, ancillary, professional and alternative health programs. Thus, key stakeholders must deliberate about how best to deploy capital so that a convenient, well-operated, efficient facility is envisioned in stages responsive to clinical innovation, regulatory changes, market demand and financial risks. Gaining support from payers, clinicians, and local employers is essential to launching a micro-hospital that’s sustainable. ERDMAN works with key clinical and administrative leaders to build a shared vision about the role and scope of the micro-hospital’s contribution to the system’s mission, vision and values.
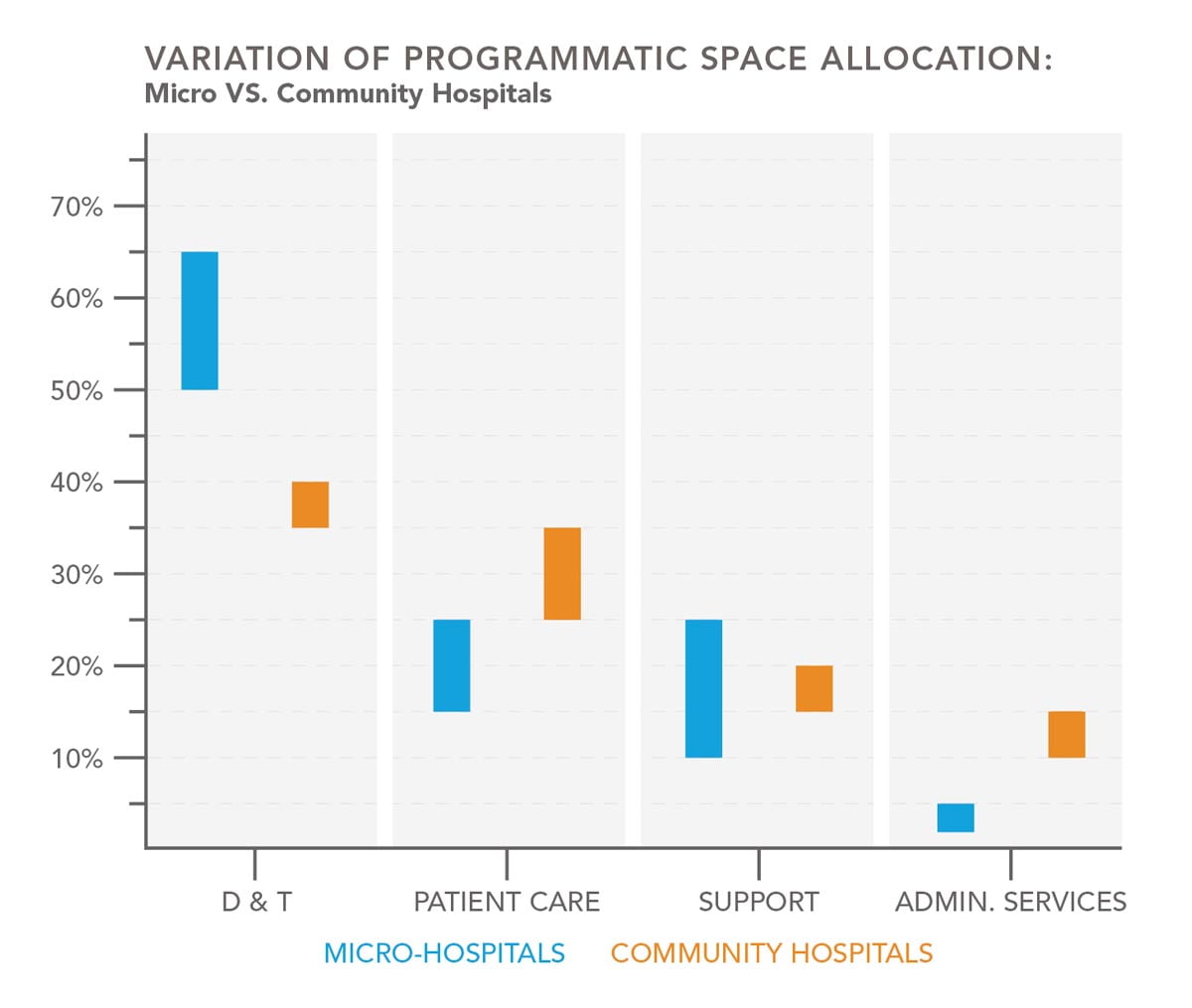
- Informed Design: With a plan in hand, sponsors must actualize the facility around precise assumptions of work-flow, patient access and use, and allowance for changes. Considerations must include clinical quality and safety requirements, staffing and workforce access, licensing and performance, and integration with digital and home-based technologies, and much more. To do this effectively, micro-hospitals cannot be looked at as scaled-down or derivative concepts of a community hospital. The featured graph represents the significant and fundamental differences in the programmatic allocation of space between the two models. Effective programming and planning must occur in the context of micro-hospitals being a new facility type, based on the operational and experiential model for the facility.
Variation of Programmatic Space Allocation: Micro vs. Community Hospitals
ERDMAN Takeaway
Micro-hospitals are emerging as a distinct sector that offers an array of acute, ancillary and retail services, while offering a lower-cost alternative to traditional hospital-outpatient facilities. They’re an integral part of a hospital’s long-term growth strategy and part of the changing landscape in care delivery.
Contributing support provided by Kevin Meek, Senior Vice President, SitePoint Ambulatory Care Partners.
For more information, please contact us.




